Loading...
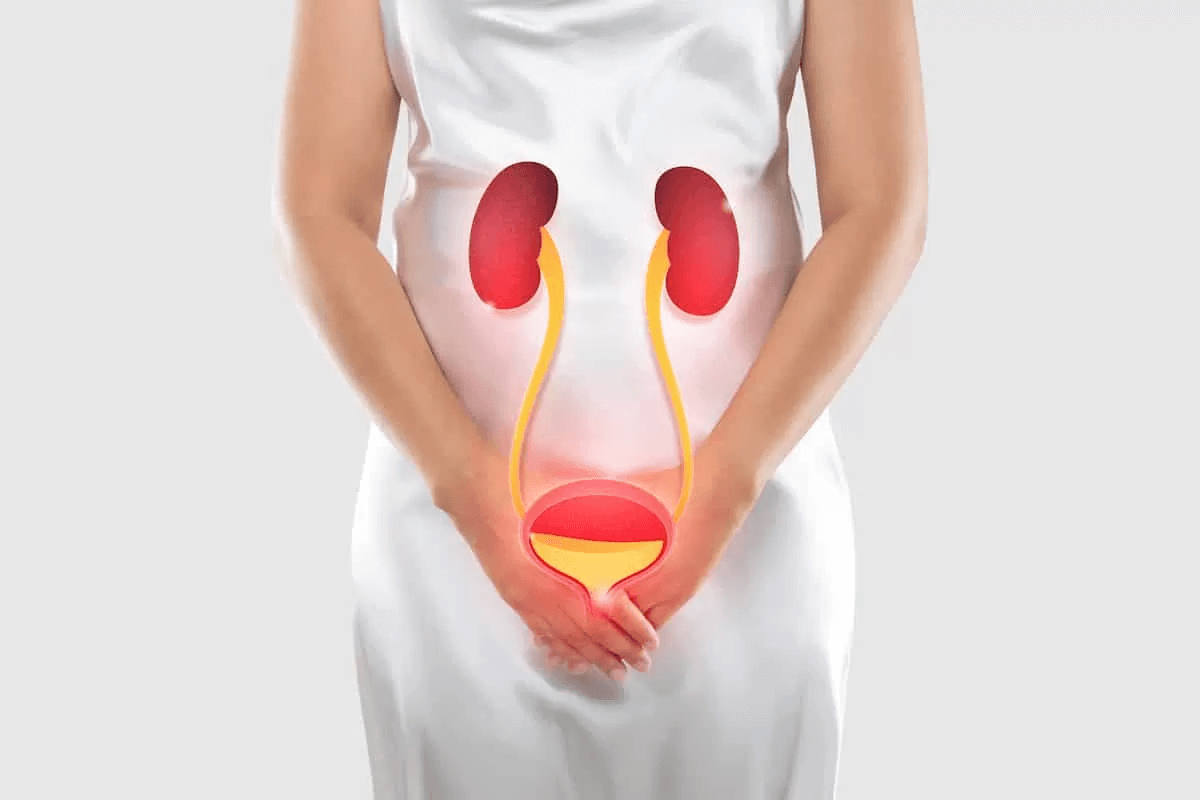
Female urology is a subspecialty of urology for diagnosis and treatment of urological conditions among females. The medical conditions arise owing to the distinctive anatomy of the female urinary tract and reproductive system.
A pediatric urologist is a surgeon trained to correct or improve congenital anomalies (birth defects) of the kidneys, bladder, ureters, or genitalia. However, several issues encountered at a pediatric urology clinic can be treated without surgery. These include some kinds of urinary incontinence, urinary tract infections, and lower grade vesicoureteral reflux.
Treating children (as patients) requires more expertise owing to the differences in adults and childrens’ ability to express and answer medical queries.
Pediatric urologists are surgeons who can diagnose, treat and care for infant and children’s urinary and genital problems.
The most common health issue seen by pediatric urologists is a urinary tract infection (UTI). These happen more often in girls than in boys.
What is a vesicovaginal fistula (VVF)?
A vesicovaginal fistula is a hole between the bladder and vagina. Depending on the size of the hole, the urine will drain continuously out the vagina, requiring multiple pullups or pads.
How does a VVF occur- In the US, the most common cause for a VVF is bladder injury that occurs during a hysterectomy (uterus removal). Bladder injuries most
commonly occur during open abdominal hysterectomies, followed by laparoscopic assisted vaginal hysterectomies. Bladder injury during a vaginal hysterectomy is very uncommon.
How is a VVF surgically repaired- There are two main methods of repairing VVF through surgery – one through the vagina and the other through an incision in the abdomen.
Most VVF can be repaired through a vaginal incision. If the hole is large, a pad of fat from the side of the vagina can be harvested and sown as a patch to the fistula. This fat pad is called a “Martius flap” and harvesting it requires a separate incision on the side of the vagina. If the fistula is also the result of pelvic radiation, a muscle from the leg can be rotated off the leg and into the vagina to act as a patch.
Fistulas that are very high in the vagina and/or close to the ureter in the bladder often require an abdominal approach because the hole may be difficult to reach through the vagina. If the ureter is involved, it may need to be resewn to the bladder – which is much easier to perform via the abdomen. If the VVF is repaired through an abdominal incision, the fistula is sewn closed. The fistula is also patched with a fat pad taken from the stomach.
How is a ureterovaginal fistula (UVF) repaired- A UVF is usually repaired by cutting the ureter and resewing it to the bladder. In select cases, a stent (plastic tube) can be placed via the bladder up the cut end of the ureter and into the kidney. If this stent can be placed, the UVF will often heal.
Stress incontinence in women can cause frequent involuntary release of urine during activities that put pressure on your bladder, such as coughing or laughing. The tension- free vaginal tape (TVT) procedure is designed to provide support for a sagging urethra so that when you cough or move vigorously or suddenly, the urethra can remain closed with no accidental release of urine.
In TVT surgery, a mesh tape is placed under your urethra like a sling or hammock to keep it in its normal position. The tape is inserted through tiny incisions in your abdomen and vaginal wall. No sutures are required to hold the tape in place. TVT surgery takes about 30 minutes and may be done under local anesthesia so you can cough at the surgeon’s request to test the tape’s support of your urethra. Other sling surgeries are done in a way that is similar to TVT surgery. Transobturator tape (TOT) surgery is done almost as often as TVT in a slightly different way.
Why is it done – Tension-free vaginal tape is used to correct stress incontinence caused by sagging of the urethra. It is a relatively simple procedure that can be done with minimal hospitalization and recovery time.
Risks – The most common risks of TVT surgery are:
✓ Injury to the bladder or urethra (perforation).
✓ Difficulty urinating after surgery.
Bladder injury and problems urinating after surgery are less common with TOT surgery. But TOT surgery has other risks including:
✓ Groin pain after surgery.
✓ Numbness or weakness in the groin or legs.
There is also a risk of problems caused by the mesh tape used in the surgery. These can include wearing away of the tissue in the pelvis. All surgeries carry some risk of infection or other complications.
The use of botulinum toxin injections to treat neurogenic detrusor overactivity (NDO) and Overactive bladder (OAB). Various neurologic conditions may cause detrusor overactivity and urinary incontinence. In select conditions, such as spinal cord injury, the attendant risk of upper tract deterioration exists as a result of pyelonephritis and increased intravesical pressure as a result of poor bladder compliance and detrusor sphincter dyssynergia.
Nerves in the body control how the bladder stores or empties urine, and problems with these nerves cause overactive bladder (OAB), incontinence, and underactive bladder (UAB) or obstructive bladder, in which the flow of urine is blocked.
Treatment-
Neurogenic bladder is a serious condition, but when it is watched closely and treated the best way, patients can see large improvements in their quality of life.
Specific treatment for neurogenic bladder will be decided by your healthcare provider based on:
✓ your age, overall health and medical history
✓ the cause of the nerve damage
✓ the type of symptoms
✓ the severity of symptoms
✓ your tolerance for certain drugs, procedures or therapies
✓ their expectations for the course of the condition

The most common surgery for prolapse is a pelvic floor repair, which is a broad term used to describe simple surgical repairs of the pelvic floor. More specifically, the term anterior repair refers to correction of the front wall of the vagina; and posterior repair refers to correction of the back wall of the vagina.
Treatment A moderate or severe cystocele may require reconstructive surgery to move the bladder into a normal position. There are a number of ways to perform this surgery, including an anterior repair. In an anterior repair, an incision (cut) is made in the wall of the vagina and the tissue that separates the bladder from the vagina is tightened. Another option, for more severe prolapse, is to place a synthetic material with a robotic or laparoscopic approach through the abdomen. This method may give more support to the tissue and help prevent the condition from happening again.
Bedwetting: A common problem is slightly more common in boys than in girls. In some young children, daytime wetting may also happen. These accidents could be a sign of a UTI or some other issue that has to do with the urinary tract.
Undescended testicles: Found in about 3 or 4 out of 100 newborns . About half of these testicles will drop on their own during the first three months of life. About 1 or 2 out of 100 boys with undescended testicles will need extra care in home and with doctors.
Vesicoureteral reflux (VUR): A health problem in which urine travels backward from the bladder toward the kidney..
About three-quarters of children treated for VUR are girls.
Hernia: Occurs when a section of intestine protrudes through a weak spot in the stomach muscle. In children, a hernia often occurs around the belly button or in the groin area.
Prenatal Hydronephrosis: A swelling of the kidney due to a backup of urine. This health issue is the most common defect found on ultrasounds during pregnancy.
Dr Rahul yadav is specialised in URS/Mini PCNL, Uretero-Pelvic Junction Obstruction (UPJO) surgery, Posterior urethral valve (PUV) incision, surgery for Undescended Testis and Vesico-ureteric reflux (VUR), Circumcision, Meatotomy, Meatoplasty.
✓ URS/Mini PCNL
✓ Uretero-Pelvic Junction Obstruction (UPJO) surgery
✓ Posterior urethral valve (PUV) incision
✓ Surgery for Undescended Testis and Vesico-ureteric reflux (VUR)
✓ Circumcision
✓ Meatoplasty